Glycation Dangers
- Thomas P Seager, PhD

- Dec 11, 2025
- 8 min read
High blood glucose causes internal injury
Summary
Glycation is the process by which blood glucose attaches itself to proteins like hemoglobin or lipoproteins like cholesterol, altering their function in the body by converting them to Advanced Glycation End products (AGEs).
Healthy blood glucose levels result in low levels of glycation, whereas blood glucose spikes result in high levels. For example, HbA1c is a measure of glycation of hemoglobin protein in the blood, and is associated with frequent episodes of elevated blood glucose.
Only glycated cholesterol is associated with heart disease. Therefore, it is not cholesterol itself that requires careful management, but blood glucose levels.
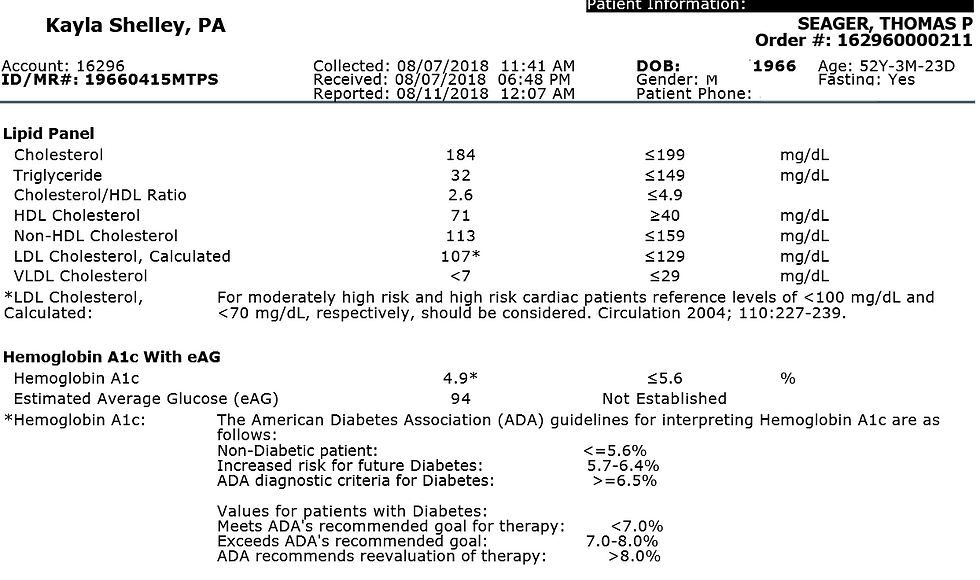
Elevated blood glucose results from insulin resistance -- the tendency of cells to reject glucose import to protect damaged mitochondria. A triglyceride/HDL ratio above 2.0 indicates insulin resistance. Below 1.0 indicates healthy insulin sensitivity.
When high cholesterol results from a ketogenic diet, blood glucose will remain low, and there is no elevated risk of heart disease.
What is glycation?
During episodes of elevated blood glucose (sometime called excursions), some of the excess glucose in the bloodstream will attach itself to proteins like hemoglobin, lipoproteins like cholesterol, and the phospholipids that make up cell membranes, creating new molecules called Advanced Glycation End products (AGEs) that have different chemical properties than the underlying proteins and lipoproteins from which they are formed.
AGEs have been observed "in all living systems surveyed so far" (Trujillo & Galligan 2023). Presumably, low levels of AGEs perform some useful function in the body, such as promoting or inhibiting cell proliferation. However, high levels of AGEs are associated with a myriad of poor health outcomes including heart disease, neuropathy, cognitive decline, metabolic dysfunction, and all the chronic illnesses associated with aging (Uceda et al. 2024). That is, the disruption of protein, lipoprotein, and phospholipid function as AGEs is one of the physiological mechanisms by which insulin resistance is the origin of every leading cause of death from chronic illness in the United States.
Glycation and cholesterol
One of the most infamous frauds in medicine is the diet-heart hypothesis invented by Ancel Keyes, PhD in response to President Dwight Eisenhower's 1955 heart attack. Rather than blame the President's habit of smoking five packs of cigarettes a day, Keys claimed that elevated blood cholesterol was the cause.
Eisenhower was the US Army General who led the successful war effort against Nazi Germany in World War 2, and Keys who developed a ready-to-eat set of meals for the soldiers called "K-rations" (presumably named "K" for "Keyes") that were packages in cans and waxed cardboard boxes obtained from the Cracker Jack candy company: :
By the late 1930s, Ancel Keys was already a respected scientist, involved in studies of nutrition and energy metabolism. His expertise in quantitative physiology from the high-altitude expedition was well recognized. At the beginning of the war, the US War Department asked him to create a nonperishable, ready-to-eat food ration with a high caloric density that could be easily carried by parachute troops. After various trials combining palatability psychology, nutritional physiology and food biochemistry and testing it on soldiers, the K ration was born, composed of three separate box-meal units: breakfast, dinner (today's lunch) and supper. Keys designed it to be used only for short durations, to avoid starvation in situations of emergency, but its use was later extended (and misused) to feed thousands of soldiers over longer periods of time on the World War II front. It is interesting to note that each meal unit contained a pack of four cigarettes, which may have been useful for the morale of the troops, but certainly not helpful from a metabolic health point of view. - Montani (2020)
K-rations had the effect of habituating American soldiers to two things: 1) ultra-processed foods, and 2) smoking tobacco. They were a tremendous boon to what eventually became multinational, multibillion-dollar processed food/tobacco oligopolies like RJR/Nabisco. However, when it was time to make heart-healthy recommendations to President Eisenhower, did Keys tell him to stop smoking? Or to eat only fresh, minimally processed foods?
Of course not.
Keys blamed the saturated fat found in meat and milk, and suggested that the unsaturated fats in ultra-processed seed oils were healthier. Although the sources of these oils were cotton seed, soybeans, rapeseed (renamed Canola), and corn, Keys renamed the seed oils as "vegetable" oils to support the impression that they were healthier, and ignored the role of cigarette smoking.
We now know that Keys' diet-heart hypothesis is wrong, and the support Keys gave when he first put it forth was fabricated by excluding data that was unfavorable to the processed foods industry. In his article series for Cross-Fit, Dr Tim Noakes has published a concise review of how Keys perpetrated the fraud, and reveals that the real origin of heart disease was always insulin resistance.
Insulin resistance
Aging is a function of mitochondrial injury
In my podcast on the Thermodynamics of Life, I explained that life is the structured flow of negentropy, or negative entropy -- also called exergy, or the thermodynamic capacity to perform work.
It is the mitochondria that channel that structure that negentropy. Mitochondria convert metabolites like glucose and fats into ATP to fuel almost every process in the body, including growth, wound repair, and movement. The mitochondria are what keep us warm by producing heat (i.e., infrared light) inside our cells. As I wrote in Cold Makes Vitamin D, the mitochondria even produce ultraviolet light in sufficient quantities to convert cholesterol into previtamin D inside our brown fat cells.
Mitochondria are life.
Unfortunately, mitochondria are also vulnerable to damage. Although they can handle a lot of stress, if they don't get periods to recover and regenerate, their energetic function will degrade. We typically call this aging, when it is really the accumulation of decades of poor mitochondrial care.
For example, in Why Is Testosterone So Low? I wrote that mitochondrial damage is responsible for the epidemic of low testosterone that seems to have engulfed America's use. Because all sex steroids originate inside the mitochondria, a gradual decay of mitochondrial function over time results in declining testosterone levels. However, when young men are exposed to environmental toxins, or persistent non-native electromagnetic frequencies (nnEMF), or eat too many seed oils, or snack incessantly on carbohydrates without ever entering ketosis, they damage their mitochondria prematurely and exhibit symptoms like low total testosterone that wouldn't otherwise appear for decades.
The mitochondria are so critical to maintenance of life, that the human body has defense mechanisms in place to protect the mitochondria from overwork. One of those is insulin resistance.
By refusing entrance of blood glucose into the cell, the mitochondria are protected from the inevitable damage that results from processing too much glucose, too fast. As hazardous as high blood glucose can be, the body seems to respond to mitochondrial injury by keeping excess glucose in the bloodstream instead of allowing it to enter the cell where processing by mitochondria could cause production of reactive oxygen species (ROS) that destroy mitochondrial DNA.
Insulin resistance and hyperglycemia kills a body slowly, while mitochondrial damage could kill a body fast.
Triglyceride to HDL ratio is a reliable blood marker
Every standard blood lipid profile reports both triglycerides (TG) and high density lipoprotein (HDL, called the good cholesterol) but few bother to compute their ratio. A high ratio above 2.0, is reliable indicator of insulin resistance, whereas a low value below 1.0 indicates excellent insulin sensitivity.
For decades, scientists have understood that his one blood marker is associated with increased risk of ischemic heart failure (Jeppesen et al 2001), dyslipidemia, metabolic syndrome, and death from cardiovascular disease. Yet, few physicians bother to track it in their patients. Current practice is to obsess with LDL cholesterol, or the very fins (smaller, denser) fraction of LDL, or ApoB -- all comparatively irrelevant indications of disease risk, but indications for prescribing profitable and dangerous statins. In other words, most physicians are not looking at their patients labs for markers of health risk, they're looking for reasons to prescribe pharmaceuticals.
As I wrote in a number of articles related to ice baths for diabetes, one of the best ways to reduce your TG/HDL ratio and thus improve your insulin sensitivity is a regular practice of cold plunge therapy. Because the cold stimulates mitobiogenesis, recruits new brown fat, and clears glucose from the blood stream, it's one of the best Mitochondrial Therapies. Even people you eat a healthy diet, get plenty of exercise, and manage their nnEMF exposure have reported improvements in TG/HDL ratio after starting a regular ice bath practice.
HbA1C - the marker of glycation
When my son was diagnosed with Type 1 diabetes, one of the blood markers his endocrinologists tracked was called HbA1c. It measures the fraction of hemoglobin in his blood that has been glycated, and thus it is an indication of the extent to which he has been experiencing blood glucose spikes during the the last three months.
In his case, because his body no longer made insulin, his blood glucose might get high because we failed to inject him with enough exogenous insulin to match his carbohydrate (and to a lesser extent, protein) intake. Those blood glucose "excursions" would cause excess glycation, and once the hemoglobin becomes attached to glucose, that attachment will never reverse. To remove the HbA1c, the red blood cell has to die and be replaced with new. Thus, an elevated HbA1c can take months to come down to healthy levels, even when my son keeps his blood glucose in good control.
After I started ice bathing every day to shrink my prostate, I measured my HbA1c at 4.9%, which is excellent. A value below 5% indicates that blood glucose excursions are infrequent. What's more, the ice baths improved my TG/HDL ratio to 0.45, which indicates outstanding insulin sensitivity.
What no doctor every told me is that hemoglobin is not the only protein to become glycated and converted to AGEs. That is, when my son measured for high HbA1c, that also meant that other proteins, lipoproteins, and phospholipids in his body were also glycated, even though they weren't being measured.
HbA1c is a proxy measure for AGEs in general. When HbA1c is too high, so are all the other AGEs, and risk of cardiovascular disease is also elevated (Bansal et al. 2023). Moreover, chronic oxidative stress amplifies those risks.
It was Brigham Young University Professor Paul Reynolds who pointed out to me that it is not cholesterol that is associated with increased risk of cardiovascular disease -- it is only that fraction of cholesterol that is glycated. The very fine cholesterol particles are the first to glycate during a blood glucose excursion, which is why they have received more attention. And when glycation is combined with oxidation, those particles become particularly dangerous.
One of the important implications of Prof. Reynold's explanation is that high cholesterol is not dangerous, until it is combined with high blood sugar and/or chronic oxidative stress. For example, a ketogenic diet can elevate cholesterol, which will sometimes alarm physicians who fail to understand the real relationship between LDL and heart disease. However, ketosis typically improves insulin sensitivity, leads to lower blood glucose levels, and mitigates chronic oxidative stress. That means that a ketogenic diet is heart-healthy because the real culprit in heart disease is not cholesterol, but insulin resistance.
References
Bansal S, Burman A, Tripathi AK. Advanced glycation end products: Key mediator and therapeutic target of cardiovascular complications in diabetes. World Journal of Diabetes. 2023 Aug 15;14(8):1146.
Jeppesen J, Hein HO, Suadicani P, Gyntelberg F. Low triglycerides–high high-density lipoprotein cholesterol and risk of ischemic heart disease. Archives of internal medicine. 2001 Feb 12;161(3):361-6.
Montani JP. Ancel Keys: The legacy of a giant in physiology, nutrition, and public health. Obesity Reviews. 2021 Mar;22:e13196.
Trujillo MN, Galligan JJ. Reconsidering the role of protein glycation in disease. nature chemical biology. 2023 Aug;19(8):922-7.
Uceda AB, Mariño L, Casasnovas R, Adrover M. An overview on glycation: molecular mechanisms, impact on proteins, pathogenesis, and inhibition. Biophysical Reviews. 2024 Apr;16(2):189-218.


In Build Now GG, I tried defending low ground for an entire match and learned how strong smart positioning really is. Winning without height felt extra satisfying.